IAOMT Oral Comments for NTP BSC
Hello, I am Dr. Jack Kall, a practicing dentist for 46 years. I am the Executive Chair of the Board of Directors of the International Academy of Oral Medicine and Toxicology, or IAOMT. We are a non-profit organization founded in 1984.
Our 1500 members are dentists, physicians and researchers who investigate and communicate safe, science-based treatments to promote whole body health. Our motto is “Show Me The Science”.
Much of our Academy’s focus has been on the toxicology of materials used in dentistry. We are the largest organization devoted to this. We have especially focused on three commonly used toxic materials in dentistry:
- mercury, a neurotoxin, used in amalgam fillings
- bisphenol A, an endocrine disrupter, used in sealants and composite fillings
- fluoride used in rinses, toothpaste, varnishes, cements and filling materials
These are all put directly into the mouth. Additionally, fluoride is used in modalities of direct ingestion in the form of fluoridated drinking water, fluoridated salt, and fluoride supplements.
For over 30 years our organization has been sponsoring and funding research on fluoride’s toxicity. We have been especially interested and very concerned about recently published studies regarding the neurotoxicity of fluoride and therefore support the NTP’s systematic review.
We are disappointed that fluoridation-promoting dental interests both within the federal government and outside it, have been trying to influence the NTP’s findings, not based on science, but in an effort to defend their policy of promoting water fluoridation.
What are the NTP’s key findings?
- That human epidemiological evidence supports a conclusion of “moderate confidence” that fluoride is a developmental neurotoxin. (BSC WG report page 342)
- That no safe exposure threshold was found for fluoride’s effect on IQ. (BSC WG report pages 87, 326, 327, 632, 703, 704)
- That fluoride exposures experienced by pregnant women and children in the US today are within the range where human studies have found reduced IQ. (BSC WG report pages 25, 26)
The report provides extensive detail on the over 150 human studies identified as relevant.
The report used rigorous, pre-established methods to rate the quality of individual studies.
The IAOMT agrees with the NTP conclusions.
We believe the monograph should have been published on its intended public release date of May 18, 2022. The revisions NTP made subsequent to it being blocked by fluoridation-promoting divisions within HHS, and the revisions suggested by the BSC working group will not alter the key findings. Any additional delays in declaring the report final are unjustified.
The IAOMT hopes the BSC will support the incredible effort that the NTP scientific experts have put into this systematic review. We agree with the external peer-reviewers who offered these comments:
“what you have done is state-of-the-art”
“the analysis itself is excellent, and you thoroughly addressed comments”
“Well done!”
“Findings… were interpreted objectively”
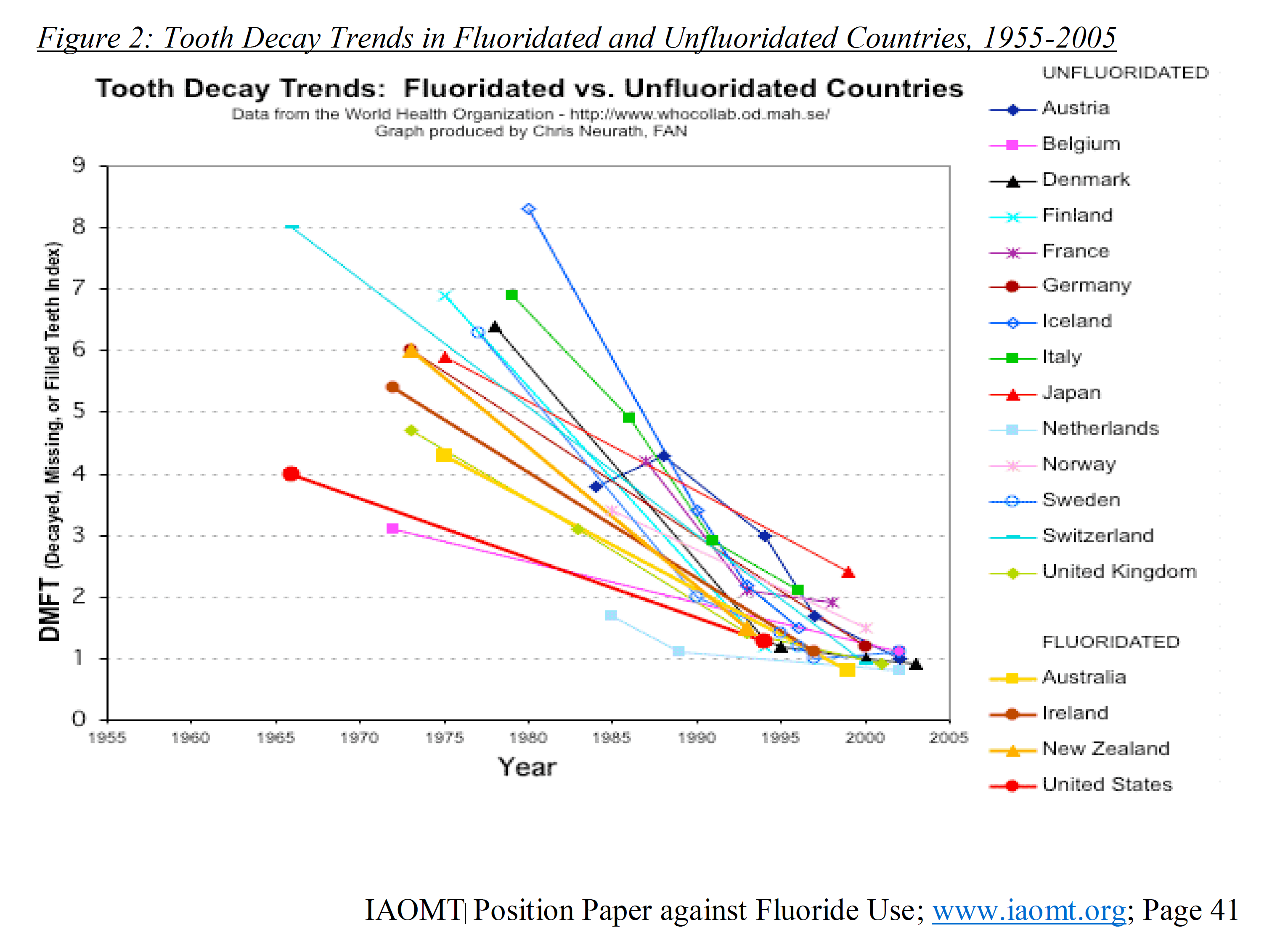
From careful review of the evidence on the association between fluoride and dental caries (tooth decay), the IAOMT has concluded the effectiveness is greatly overstated for today’s oral health situation. Countries with fluoridation and those without have both experienced the same dramatic declines in tooth decay over the past 50 years, as shown in this graph based on WHO data:
The most recent large-scale community fluoridation trial, done in England, found only a difference of 0.2 cavities per child in baby teeth. It found no statistically significant benefit at all in permanent teeth. The study was commissioned by Public Health England, the leading promoter of fluoridation in England. Yet the study’s authors even concluded that the benefits “are much smaller than earlier research suggested” and that fluoridation did not shrink dental health inequalities between poorer and wealthier children.
Even the US CDC acknowledges there is no evidence that prenatal fluoride in the pregnant mother or in the infant before teeth have erupted provides any dental benefit. These are precisely the exposure periods where the evidence for developmental neurotoxicity is strongest.
A cornerstone of public health policy known as the precautionary principle must be considered as well. The basic premise of this policy is built upon the centuries-old medical oath to “first, do no harm.” Yet, the modern application of the precautionary principle is actually supported by an international agreement.
In January 1998, at an international conference involving scientists, lawyers, policy makers, and environmentalists from the U.S., Canada and Europe, a formalized statement was signed and became known as the “Wingspread Statement on the Precautionary Principle.”530 In it, the following advice is given: “When an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause and effect relationships are not fully established scientifically. In this context the proponent of an activity, rather than the public, should bear the burden of proof.”
Not surprisingly, the need for the appropriate application of the precautionary principle has been associated with fluoride usage. Authors of a 2006 article entitled “What Does the Precautionary Principle Mean for Evidence-Based Dentistry?” suggested the need to account for cumulative exposures from all fluoride sources and population variability, while also stating that consumers can reach “optimal” fluoridation levels without ever drinking fluoridated water. Additionally, researchers of a review published in 2014 addressed the obligation for the precautionary principle to be applied to fluoride usage, and they took this concept one step further when they suggested that our modern-day understanding of dental caries “diminishes any major future role for fluoride in caries prevention.”
I close with the IAOMT’s position on fluoride:
“In summary, given the elevated number of fluoride sources and the increased rates of fluoride intake in the American population, which have risen substantially since water fluoridation began in the 1940’s, it has become a necessity to reduce and work toward eliminating avoidable sources of fluoride exposure, including water fluoridation, fluoride containing dental materials, and other fluoridated products.”
Fluoride Article Author
Dr. Jack Kall, DMD, FAGD, MIAOMT, is a Fellow of the Academy of General Dentistry and a past President of the Kentucky chapter. He is an Accredited Master of the International Academy of Oral Medicine and Toxicology (IAOMT) and since 1996 has served as the Chairman of its’ Board of Directors. He also serves on the Bioregulatory Medical Institute’s (BRMI) Board of Advisors. He is a member of the Institute for Functional Medicine and American Academy for Oral Systemic Health.



