Included within Appendix IV is a table containing over 150 references describing illness associated with the use of amalgam fillings. It is only a small subset of the available literature. From that table newer epidemiological studies that have been conducted since the 2019 FDA report, Epidemiological Evidence on the Adverse Health Effects Reported in Relation to Mercury from Dental Amalgam: A systematic literature (2010 – Present) was released in September 2019, are presented in more detail below.
Bilak, Ş, M. Önderci, and A. Şimşek. “Evaluation of Amalgam-Related Retinal Neurotoxicity with Optical Coherence Tomography Findings.” Human & Experimental Toxicology 38, no. 7 (July 2019): 814–22. https://doi.org/10.1177/0960327119842637.
Bilak et al (2019) evaluated the neurotoxic effect of amalgam dental fillings on plasma mercury (Hg) levels and retino-choroidal layers using spectral domain optical coherence tomography (SD-OCT). Participants were 56 individuals with amalgam dental fillings and 44 individuals without. All individuals participated in detailed ophthalmic and oral examinations. Venous blood samples were collected, and blood Hg levels were measured. Correlations between SD-OCT measurement results and blood Hg levels were analyzed.
RESULTS: There were no differences between groups in age, sex, or body mass index. The mean blood Hg level was 2.76 ± 1.21 µg/L in the amalgam group and 2.06 ± 1.15 µg/L in the control group (p = 0.04). The Hg/BMI ratio was 0.12 ± 0.06 kg/m2 in the amalgam group and 0.09 ± 0.05 kg/m2 in the control group (p = 0.01). Reduced volumes of ganglion cell layer and inner plexiform layer were observed in the amalgam group when compared with the control group (p < 0.05).
CONCLUSION: Amalgam dental fillings can cause retinal neurotoxicity.
Björkman, Lars, Gunvor B. Lygre, Kjell Haug, and Rolv Skjærven. “Perinatal Death and Exposure to Dental Amalgam Fillings during Pregnancy in the Population-Based MoBa Cohort.” PloS One 13, no. 12 (2018): e0208803. https://doi.org/10.1371/journal.pone.0208803.
The aim of this population-based observational cohort study conducted by Björkman and colleagues (2018) was to compare the risk of perinatal death in mothers bearing amalgam fillings compared to those without. Data were acquired from The Norwegian Mother and Child Cohort Study, a birth cohort of children born in 1999-2008 conducted by the Norwegian Institute of Public Health. The sample was comprised of 72,038 pregnant women with data on the number of teeth filled with dental amalgam. Data on perinatal death (stillbirth ≥ 22 weeks plus early neonatal death 0-7 days after birth) were obtained from the Medical Birth Registry of Norway.
RESULTS: The absolute risk of perinatal death ranged from 0.20% in women with no amalgam-filled teeth to 0.67% in women with 13 or more teeth filled with amalgam. Correlational analyses showed that increased risk of perinatal death correlated with the number of teeth filled with dental amalgam (p<0.001). After adjustment for potential confounders (mothers’ age, education, body mass index, parity, smoking during pregnancy, alcohol consumption during pregnancy) there was still an increased risk for perinatal death associated with increasing number of teeth filled with amalgam (p = 0.015).
CONCLUSION: The current findings suggest that the risk of perinatal death could increase dose-dependently depending on the mother’s number of amalgam filled teeth.
Duplinsky, Thomas G., and Domenic V. Cicchetti. “The Health Status of Dentists Exposed to Mercury from Silver Amalgam Tooth Restorations,” 2012. https://doi.org/10.6000/1929-6029.2012.01.01.01.
[This is an older article but was omitted from the FDA 2019 Epidemiological Report]The purpose of this investigation was to compare the health status of general practice dentists with matched controls, in five disease categories: Neuropsychiatric, neurologic, combined neuropsychiatric and neurologic, respiratory and cardiovascular disorders. Pharmacy utilization data was used to evaluate the health status of a representative sample of 396 dentists, and 708 control subjects, matched on age, geographical area, and insurance plan structure. All subjects were male.
RESULTS: Dentists demonstrated significantly more prescription utilization (PU) of specific illness medications than did controls, for all 5 disease categories (see Table)
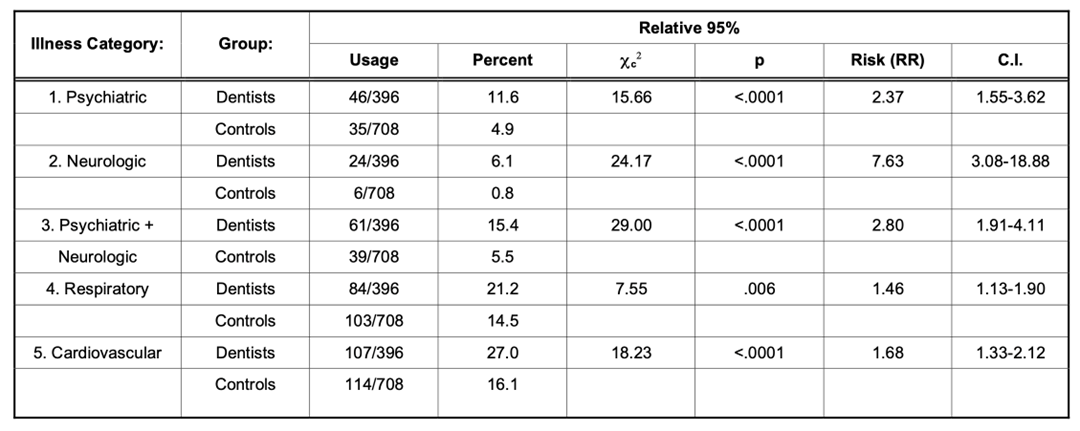
CONCLUSION: Over half of pediatric and general practice dentists still use mercury amalgam restorations placing them at greater risk than the general population for those disorders, as well as threatening the future health of America’s children and adults who continue to receive silver amalgam restorations.
Geier, David A., and Mark R. Geier. “Dental Amalgams and the Incidence Rate of Arthritis among American Adults.” Clinical Medicine Insights. Arthritis and Musculoskeletal Disorders 14 (2021): 11795441211016261. https://doi.org/10.1177/11795441211016261.
This study conducted by Geier and Geier (2021) examined the relationship between mercury (Hg)-based dental amalgams and arthritis diagnoses among adults in the US. 86,305,425 weighted-persons with ⩾1 dental amalgam filling surface (exposed group) and 32,201,088 weighted-persons with ⩾1 other dental filling surface (unexposed group) were examined in the 2015-2016 National Health and Nutritional Examination Survey (NHANES). All persons were 20-80 years-old with known demographic characteristics and arthritis status. Survey logistic regression and survey frequency modeling were employed with and without adjustment of covariates.
RESULTS: The arthritis rate was significantly greater in the exposed group compared to the unexposed group in the unadjusted (7.68-fold) and adjusted (4.89-fold) models. Arthritis (per 10 000 weighted-person-years) was 6.0-fold greater in the exposed group (6.2) compared to the unexposed group (1.06). A significant bimodal dose-dependent relationship between Hg exposure and arthritis rate was observed. The arthritis rate increased with increasing exposure (peak among persons with 4-7 amalgam fillings) and, subsequently, decreased among those with >6. A significant decrease in arthritis rate among persons with >13 amalgams as compared to those persons with 4-7 was observed. A significant association between amalgams and arthritis risk and a dose-dependent amalgam-associated immune-stimulation/immune-suppression with arthritis risk were observed.
CONCLUSIONS: An estimated additional $96,835,814 US dollars are spent on annual medical costs and $184,797,680 are lost in annual wages, amounting to total annual costs of $281 633 494 from reported new onset arthritis associated with amalgam fillings.
Geier, David A., and Mark R. Geier. “Reported Asthma and Dental Amalgam Exposure among Adults in the United States: An Assessment of the National Health and Nutrition Examination Survey.” SAGE Open Medicine 9 (2021): 20503121211048677. https://doi.org/10.1177/20503121211048677.
This hypothesis-testing study conducted by Geier and Geier (2021) evaluated the relationship between dental amalgam exposure and the risk of reported asthma diagnoses in American adults. 97,861,577 weighted-persons with ⩾1 dental amalgam surfaces (exposed group) were compared with 31,716,558 weighted-persons ⩾1 other dental surfaces (no dental amalgams, unexposed group) using the 2015-2016 National Health and Nutrition Examination Survey (NHANES). All persons were 20-80 years old and with known reported asthma status (only newly diagnosed asthma cases were examined). Logistic regression and survey frequency modeling were employed to evaluate the relative incidence rate of reported asthma diagnoses among those in the exposed group compared to the unexposed group. Analyses controlled for gender, race, socioeconomic status, educational status, country of birth, and tobacco exposure.
RESULTS: There was a significantly increased incidence rate of reported asthma in the exposed group as compared to the unexposed group in unadjusted (4.46-fold) and adjusted (4.84-fold) models. A dose-response relationship was observed for the risk of reported asthma per dental amalgam filling surface in both models. Survey frequency modeling revealed that the frequency of reported asthma (per 10,000 weighted-person years) was 3.66-fold higher in the exposed group (2.06) compared to the unexposed group (0.56).
CONCLUSION: Increased dental amalgam exposure was associated with an increased risk of reported asthma diagnoses in American adults.
Sanders, Alison P., Matthew J. Mazzella, Ashley J. Malin, Gleicy M. Hair, Stefanie A. Busgang, Jeffrey M. Saland, and Paul Curtin. “Combined Exposure to Lead, Cadmium, Mercury, and Arsenic and Kidney Health in Adolescents Age 12-19 in NHANES 2009-2014.” Environment International 131 (October 2019): 104993. https://doi.org/10.1016/j.envint.2019.104993.
In this study, Sanders et al (2019) tested whether there was an association between co-exposure to lead (Pb), cadmium (Cd), mercury (Hg), and arsenic (As), measured in urine and blood, and kidney parameters in US adolescents. A cross-sectional analysis was conducted during 2009-2014 of a subsample of 2709 children aged 12-19 participating in the National Health and Nutrition Examination Survey (NHANES). Urines were analyzed for 4 nephrotoxic metals selected a priori (As, Cd, Pb and Hg), and bloods were analyzed for Cd, Pb, and Hg. Regression analysis using these analytes and estimated glomerular filtration rate (eGFR), serum uric acid, urine albumin, blood urea nitrogen (BUN), were made adjusting for sex, race/ethnicity, age, head of household’s education level, height, BMI, serum cotinine, and NHANES cohort year. Urines were also adjusted for creatinine, and bloods and urines were adjusted for fish consumption.
RESULTS: In regression models, each decile increase of urine heavy metals was associated with significantly higher BUN, eGFR, and urine albumin. The association between urine metals and BUN was primarily driven by As (72%), while the association with eGFR was driven by Hg (61%), and Cd (17%), and the association with urine albumin was driven by Cd (37%), Hg (33%), and Pb (25%). In regression models of combined blood metals, each decile increase was associated with 0.6% (95% CI: 0.0, 1.3) higher serum uric acid driven by Pb (43%), Hg (33%), and Cd (24%) (p = 0.05).
CONCLUSIONS: The findings suggest metals including As, Pb, Hg, Cd and their combinations may affect renal parameters, although potential reverse causation cannot be ruled out due to the cross-sectional study design. Implications of early life low-level exposure to multiple metals on kidney function may have far-reaching consequences later in life in the development of hypertension, kidney disease, and renal dysfunction. Longitudinal studies should further evaluate these relationships.
Szklarek, Magdalena, and Tomasz Kostka. “The Impact of the Use of Amalgam in Dental Treatment on the Prevalence of Restless Legs Syndrome in Older People.” Medycyna Pracy 70, no. 1 (February 28, 2019): 9–16. https://doi.org/10.13075/mp.5893.00749.
The potential relationship between restless legs syndrome (RLS) and amalgam fillings in older people was investigated in this study conducted by Szklarek et al (2019) in 41 people with RLS and 63 without, aged 60-97. By using 4 questions, together with the diagnostic criteria from the questionnaire produced by the International Restless Legs Syndrome Study Group (IRLSSG), authors assessed the occurrence and extent of symptoms of RLS. Medical/dental history and examination were used to determine dental restorative materials (i.e., amalgam or other) and the number of such fillings.
RESULTS: People with RLS symptoms had a significantly greater number of amalgam fillings compared to people without. Multiple logistic regression, controlling for age and gender, showed that the number of amalgam fillings correlated with RLS symptoms (p = 0.02)
CONCLUSIONS: The presence of amalgam fillings should be considered within individuals with RLS.
Yao, Xu, Xu Steven Xu, Yaning Yang, Zhi Zhu, Zhao Zhu, Fangbiao Tao, and Min Yuan. “Stratification of Population in NHANES 2009-2014 Based on Exposure Pattern of Lead, Cadmium, Mercury, and Arsenic and Their Association with Cardiovascular, Renal and Respiratory Outcomes.” Environment International 149 (April 2021): 106410. https://doi.org/10.1016/j.envint.2021.106410.
Environmental exposure to toxic metals is an important risk factor to human health. In the setting of ubiquitous heterogeneous environmental exposures, statistical methods that incorporate mixed exposures are increasingly relevant and may provide new insight into the association between metal exposure and important cardiovascular, renal and respiratory outcomes. The objective of the Xu et al (2021) study was to examine 12 a priori health endpoints with respect to heavy metal status. 9662 subjects participating in the 6 cycles (2003-2004 to 2013-2014) of the National Health and Nutrition Examination Survey (NHANES) were grouped into high and low toxic metal exposure groups. Lead, cadmium and arsenic levels were acquired from urine, and lead, cadmium and mercury levels were measured from blood. Analyses controlled for age, sex, race/ethnicity, education, smoking status, BMI, and urinary creatinine.
RESULTS: The concentrations of all the three heavy metals were significantly different between the identified groups in blood (p < 2.2e-16) or in urine (p = 0). The high-exposure group according to either blood or urinary metal levels had significantly higher total mortality (1.63-1.64 times higher, p < 0.0001), mortality caused by malignant neoplasms (2.05-2.62 times higher, p < 0.0002), Gamma-glutamyl transferase (GGT) (1.03-1.05 times higher, p < 0.0001). In addition, based on blood levels, the high-exposure group was associated with higher systolic blood pressure, death related to hypertension, heart disease and chronic lower respiratory disease. Based on urine levels the high-exposure group had higher mortality related to nephritis.
CONCLUSIONS: Heavy metal exposure is associated with poor health endpoints and increased mortality.


